
Fluorosis is a cowardly disease; it selectively preys upon the most vulnerable and renders them even more fragile. We have discussed earlier how fluoride contamination is especially deadly to the poor of India as they lack the nutrition, the options and the information needed to combat it. Within that vulnerable community lies another group that is extremely susceptible to fluorosis. This group is extremely underserved, almost entirely dependent on external help, lacks the ability to ask for this help, lacks the ability to implement interventions on its own, and is physically more likely to contract fluorosis. Skeletal fluorosis within this group has the potential to set back the lives of entire communities.
These are the children of rural India.
Why is fluorosis more toxic for children?
The amount of fluoride that is unsafe for people depends on the weight of the person. 1 mg of fluoride, for example, might be safe for a person who weighs 50 kgs but is toxic for a child who weighs just 10 kgs. This means that what we consider to be 'safe' limits--1.0 to 1.5 mg of fluoride per litre--can be toxic for a young child whose body weight is probably 5 times lesser than that of an adult.
'Safe limits' of fluoride can be toxic for a young child whose body weight is probably 5 times lesser than that of an adult.
What is the link between fluoride and calcium deficiency?
Fluoride rapidly increases the rate of growth of bones in the body. This is contradictory to people's assumptions. It increases growth to such an extent that calcium and other bone minerals are not available, so at the end of it fluoride consumes all the calcium in the body. As a basic thumb rule, what we understand is that when 1 mg of fluoride enters the body, it takes away 40 mg of the calcium with it. So if a growing child needs around 800 mg of calcium a day, 10 mg of fluoride a day will take out 400 mg of calcium, thereby leaving them with a deficit of 400 mg.
Why are children more vulnerable than adults?
In rural India, children do not consume enough calcium. They also do not get enough of Vitamin D, magnesium, zinc, or other bone building minerals. This is especially true in remote areas where children do not consume milk. On the contrary, they begin having tea at a very young age. Tea, especially black tea, naturally contains fluoride, irrespective of where it is grown.
When the mother herself is highly deficient in micro nutrients, children already end up with a very low birth weight and added to this, very little calcium goes to the children from the mother's milk. So children have an implicit calcium deficiency which becomes greater with the consumption of fluoride whether through contaminated water or foods that are naturally high in fluoride. At the same time, their low body weight magnifies the toxicity of ingested fluoride. What this means is that children develop severe bone deformities that adults with 20-30 years of exposure to the same fluoride contamination, will not face.
Children have an implicit calcium deficiency that is worsened by fluoride consumption.
Within 2-3 years of birth, they start having bone deformities. At that age dental fluorosis isn't visible; that becomes apparent only after 6-7 years. Traveling to areas with high fluoride show many children with various deformities starting with swollen knees on the inner side, going on to bowed legs and other disabilities.
Is fluoride linked only to water?
Earlier we (INREM Foundation) thought it was just a water problem. People like Dr. A. K. Susheela, Dr. Tapas Chakma and Dr. Raja Reddy, pointed out that this was a severe malnutrition problem, not just of calcium but a host of other things too. The problem is caused by basic malnutrition and within that calcium deficiency is increased by high fluoride entering the body. The positive thing is that these are children, and acting quickly can save them. We were not convinced in the beginning but these doctors, especially Dr. Raja Reddy, persisted. He said, "You have to stop consumption of fluoride in water. The second thing is to get safe nutrition into the body".
What do we mean by safe nutrition?
We cannot pump heavy nutritional supplements into a child's body as it won't get absorbed. We need to start with better food in general. Dr. Reddy prescribed a good amount of calcium, some magnesium and then Vitamin C as the right kind of mix that can detoxify the body and strengthen the bones.
The attempts
INREM started in Jhabua in 2010. At the outset, the problem was how to reach children in remote places, and then how to convince the parents about the truth of what you are saying--a basic problem of communication. After that came the problem of making sure that safe water and good nutrition reach these children. To begin with, it was a nightmare for us. The people we were working with were away from any water supply programmes and there were no safe water sources next to them. We needed solutions that could reach their households and that they would use.

We realised that for safe water we had no option but to try a domestic fluoride removal filter although we understand that this is not sustainable in the longer term. If we could design something that was useful for these families and make them use it through a slow process of giving them behaviour support, then maybe we can do it. So that's something that we invested in--designing a simple household filter that removes flouride. Later we realised that a more sustainable option was to identify fluoride-free safe water sources and get people to use them.
Adequate nutrition
On the nutrition side we needed innovations. We know that amla (gooseberry) is the best source of Vitamin C, but how do you get it to people? We first started with drying amla and using it either salted or sweetened. But sweet amla gets over in two days; the children just eat it up. We recommended putting salted amla in dal, but some families do it and some don't. We didn't have a great experience with supplying amla in this manner. We then realised that people have a very strong affinity and expectation from tablets, so we thought of converting amla powder to tablets.
Dr.Vithalbhai Patel, an ayurvedic doctor who has now expired, agreed to try making tablets out of amla powder and he succeeded. One amla tablet contains 7-8 mg of vitamin C and that was sufficient. The tablets had a great acceptance among people. Among severely affected people, we started with supplements of calcium, vitamins D and C, magnesium and zinc which we got for a very low cost from a Chandigarh-based company but we accepted that this was not sufficient.
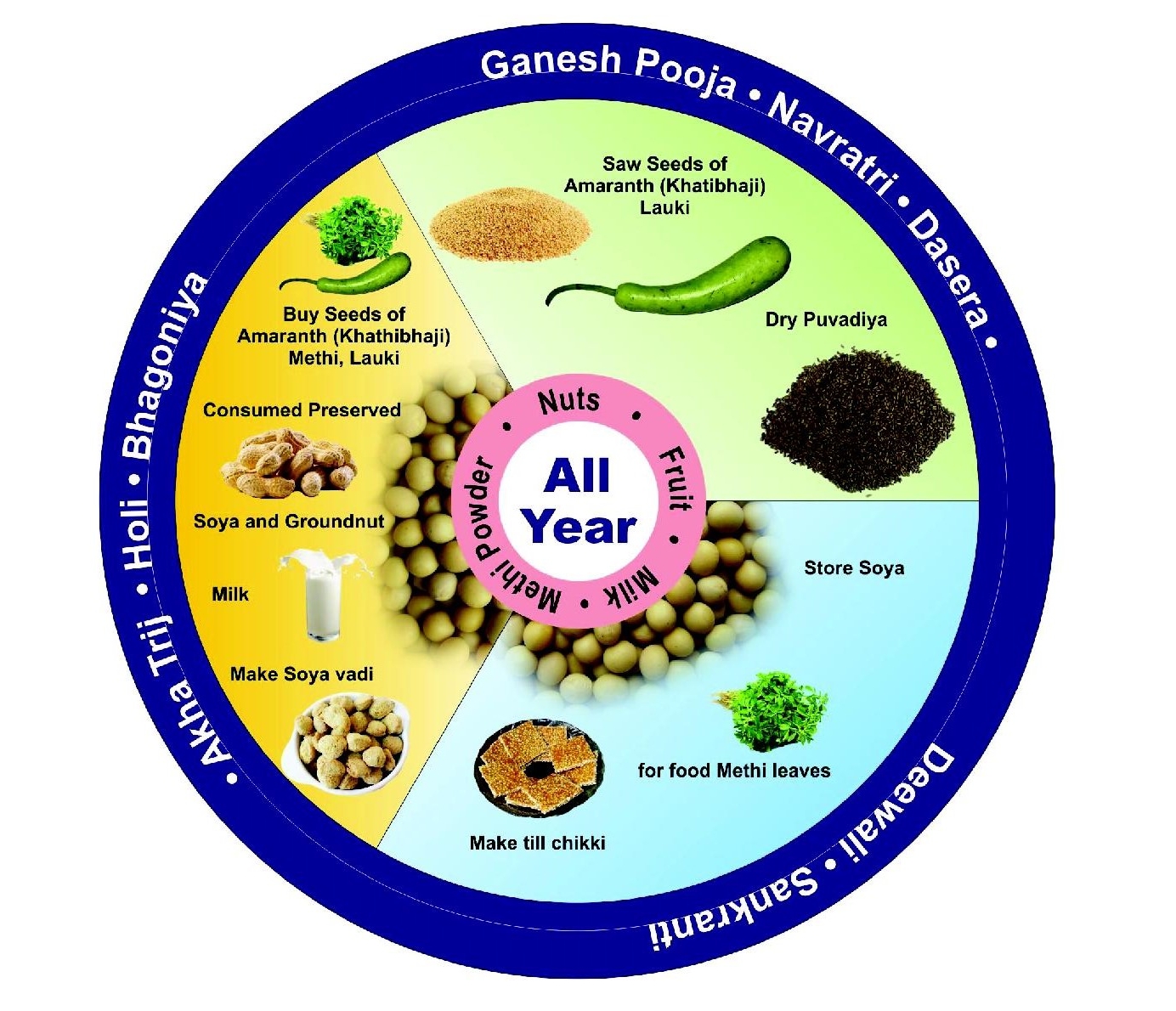
We also needed good food, especially food that can be prepared and contained calories as well as nutrients. For that, til chikki emerged as a good option. The sesame seeds and jaggery contain calcium and magnesium along with calories. This is something we focused on for the winter months. We tried with different types of food, but nothing succeeded as much as til chikki. We also tried a lot with soya based products such as soya laddoo.
The first victories
With this combination of safe water and nutrition, we found that slowly we saw recovery. The example of Nilesh is well recorded because we had taken some videos earlier and could document the visual aspect of it.
But then we also had blood, urine and x-ray measurements. And that gave us evidence over the years that the children were recovering. There were about 20-22 children with skeletal fluorosis and all of them showed recovery, some more than others. Once this started happening, more and more people started coming to us. It was a surprise that bone deformities can be cured. We still have some deformities in the children, but with the entire process we followed, these deformities slowly started going away. Legs started straightening, they got more hope, started walking and running. The same child who was walking in a crippled way was now walking much more normally. We then went out to other families out there and some of them came forward, some did not. Even after seeing this improvement, some of them did not come forward. So we wondered what is wrong, what is the mistake we are doing.
Behaviour change communication
It was a challenge to us to work with these few families and try to cure these children, but what do you do about others who are not coming forward? That's when we started focusing on different messages for communication, of both hope and threat. We would offer hope by saying that your child is going to be fine but also state that if you don't do it, this will happen and that was the threat. We needed a mix because some people responded more to threat, some more to hope. For example, when the government took out the handpumps, we thought that was not a good idea but that worked with some people. They went to safer sources and are still sticking to it after 4-5 years. We realised that we need to take the message to a wider audience.
 The campaign
The campaign
When we went around Jhabua, we realised we have to change our strategy. It is not just about the few examples of food that we recommend, we need to expand the range of food that gives a wide range of nutrients. We also need to give people an opportunity to produce locally. That is what we have been doing for the last couple of years in a campaign mode in Jhabua. We are now reaching around 20,000 people in 28 villages. That is a lot of people for a small team like us that has just three people on the field. What we did was train local drama groups on fluorosis over a period of about six months. They imbibed it so much that they now themselves communicate it to people through street dramas. That helped to take the message across to people, to say that this is the problem and this is the solution.
The options
People spend money to buy things from the market. We felt that there should be options for buying low cost nutritious food. We zeroed down on gram, eggs, jaggery, milk powder, jaggery products like chikki, and soya related products. All these have high amounts of the nutrients that we need. We promoted these things that people can buy. We are also working with people to cultivate some nutrient rich foods close to their house in a way that people also get what they want. People want tomatoes and chillies because they are tasty. We promote green vegetables like amaranth which are good for resisting fluorosis. We have been able to reach around 250 households with small nutrition gardens and 50-60 households with large nutrition gardens.
Gram, eggs, jaggery, milk powder, jaggery products and green vegetables are foods that resist fluorosis
The impact
From starting with a few children, communicating to the immediate villages, and going to mass communication to a large population, we have come a long way in these five years. But the problem is not just in Jhabua. There are a lot of children in the country who can benefit, who can avoid a life of disability. This can be done not with surgery but with safe water and good food. Also, there is a larger impact. It is not just about fluorosis, but safe water and good food can protect us from a whole host of diseases. The early stages of our life are most important. From birth to five years, safe water and good food is crucial. Stop the toxics and improve the nutrients. If you do that, you will get a generation of healthy people who can work well, be good in school, and have good livelihoods for the rest of their life. All the aspirations that people have for their lives could be achieved.
Dr. Sunderrajan Krishnan is the director of INREM Foundation, which works in areas of water, public health, agriculture and the environment. This article is a transcript of an audio file submitted by Dr. Krishnan. For ease of reading, we have made minor edits including adding sub-headings.
/articles/catch-them-young-treating-children-affected-fluorosis